Campus Epidemiology of SARS-CoV-2 Variant Infections
SARS-CoV-2, also known as COVID-19, has caused significant morbidity and mortality amongst populations globally (1). Contextually, in the United States, COVID-19 has presented a huge burden, totaling over 500,000 deaths. As the pandemic has continued, new variants of SARS-CoV-2 characterized by key mutations in the viral spike protein have been identified globally (2, 3). Recent SARS-CoV-2 cases have cited a presence of variants. The B.1.1.7(United Kingdom), B.1.351(South Africa), and the P.1(Brazil) variants have been associated with increased transmission and prevalence globally. Furthermore, some variants might have increased virulence and be associated with decreased vaccine efficacy (4, 5). Recently in Southern California, a novel SARS-CoV-2 variant (CAL.20C) was identified, different than the 20G clade, the most common clade in North America (6). However, little is known about the epidemiology of those or other variants of SARS-CoV-2 in the United States (7-9). Due to recency of variant exposure in the United States, there is not much literature citing the effects of these variants. The US Centers for Disease Control and Prevention urgently recommends sequencing more SARS-CoV-2 genomes to improve the understanding of circulating SARS-CoV-2 in terms of transmissibility, symptom severity, detection evasion, susceptibility to therapeutics, and evasion of natural or vaccine-induced immunity (10). Although it is unclear what specific variants are present in Los Angeles and what their prevalence or clinical implications might be, this study will aim to address that gap in information.
The Trojan Pandemic Response Initiative: Uptake, Markers and Determinants of Effectiveness, Subsequent Behaviors
We propose a study of the impact of the on-going SARS-CoV-2 Pandemic and Vaccination Campaign on USC students, staff and faculty that will (a) generate real-time evidence of attitudes, behaviors, and infections acutely needed for USC to pursue strategies and policies to minimize new COVID-19 infections while the USC public health campaign, including vaccinations, continues; and (b) capitalize on USC’s scientific strengths and the diversity of its workforce to generate scientific knowledge that both advances the field and is relatively unique. Leveraging an outstanding multi-disciplinary team and the ability to merge the data on individuals we will collect with their data from the on-going USC campaign of PCR testing for COVID, Trojan checks and vaccinations, we will recruit (1) 8,000 subjects into a ‘University Cohort’ that will be briefly surveyed and then followed to determine vaccine effectiveness; (2) 4,000 subjects into a ‘Survey/Health Cohort’ that will undergo intensive surveys repeated over time to ascertain the evolution of attitudes and behaviors in relation to infections and vaccinations; and (3) a ‘Biomarker Cohort’ of 600 subjects that will undergo the surveys as well as repeated collection of serum, cells, saliva, and urine in conjunction with and after their vaccinations.
SARS-CoV-2 Antibody Testing in Vulnerable Communities
Low-income residents of Los Angeles County are dying of COVID-19 at a rate nearly four times that of residents in wealthier communities. The current pandemic is magnifying existing health disparities and is creating an immediate need for increased testing, better understanding of personalized risk in low-income households, connection to health care and support services, and culturally-tailored information and recommendations. The primary goal of the study is to recruit a random sample of 2000 persons (500-1000 households) who have sought care at AltaMed Health Services (a Federally Qualified Health Center in Los Angeles), and test them for SARS-CoV-2 antibodies. A secondary objective is to integrate test results with a brief set of self-report measures on social determinants of health to predict risk of positive tests. Households are invited to complete a survey and members are offered $20 to participate in antibody testing. We will estimate the true proportion of positive tests and produce displays of the frequency distribution of positive tests as they relate to most common medical conditions and social determinants of health, caregiving responsibilities, and food access/distance needed to travel to obtain essential goods. This project will provide valuable information about those most at risk of contracting COVID-19 and will offer actionable information that may help prevent further spread of the disease.
Understanding Disparities in COVID-19 Mortality and the Role of Short- and Long-term Air Pollution Exposure

Emerging data indicate disproportionate COVID-19 death rates among members of racial/ethnic minority groups. The contribution of demographic factors, socioeconomic status (SES), population mobility, and environmental exposures is unclear. Using California death certificate data, we will study potential determinants of probable COVID-19 deaths and excess all-cause mortality during the pandemic. We will determine the contribution to race/ethnicity mortality disparities of individual level determinants (e.g., sex, age) as well as contextual factors (e.g., neighborhood SES, time-varying cell-phone based mobility). We will then evaluate independent associations of acute (prior 1-8 weeks) and chronic (prior 1-2 years) air pollution exposure with mortality. The expected outcome of this investigation is an improved understanding of the individual and contextual factors related to COVID-19 mortality. The project will also reveal the impacts of chronic and acute ambient air pollution on COVID-19 mortality. Study findings will have an important positive impact by identifying high-risk, vulnerable communities that can guide more targeted and effective public health interventions. Clarifying the role of air pollution in COVID-19 deaths could be highly relevant to air quality regulations that potentially could reduce mortality.
Impact of the COVID-19 pandemic on cancer care delivery

The Coronavirus (COVID-19) pandemic has drastically impacted cancer patients, forcing many patients to undergo sudden and unplanned changes to their cancer care. Oncologists and surgeons have had to face the difficulty of deciding how to best continue care for their patients while minimizing the risk of COVID-19 infection. The COVID-19 pandemic may have also created barriers for many patients to adhere to treatment recommendations and to deal with cancer treatment induced side effects and co-morbidities. Minority populations, specifically Blacks and Latinos across the US, are experiencing disparities in COVID-19 infections and related deaths. We fear that in addition to disparities in COVID-19 infections and deaths, the pandemic is also widening the existing cancer disparities among Blacks and Latinos. We propose to asses the impact of ongoing changes in cancer care delivery among diverse populations and to better serve cancer care patients as the pandemic continues to impact their lives. We will do this by evaluating the changes and type of care received by patients since the pandemic started, and its impact on short-term outcomes. We will also reach out to patients to administer surveys to understand the impact of COVID-19 on cancer delivery and treatment adherence. Our study will include patients diagnosed since the pandemic started at the USC Norris Comprehensive Cancer Center in Los Angeles, the University of Florida Health in Jacksonville, Florida, and the Capital Regional Cancer Center in Tallahassee, Florida. This study is done in partnership with the Florida-California CaRE2 Health Equity Center (www.care2healthequitycenter.org)
Epidemiological COVID-19 model for Los Angeles County
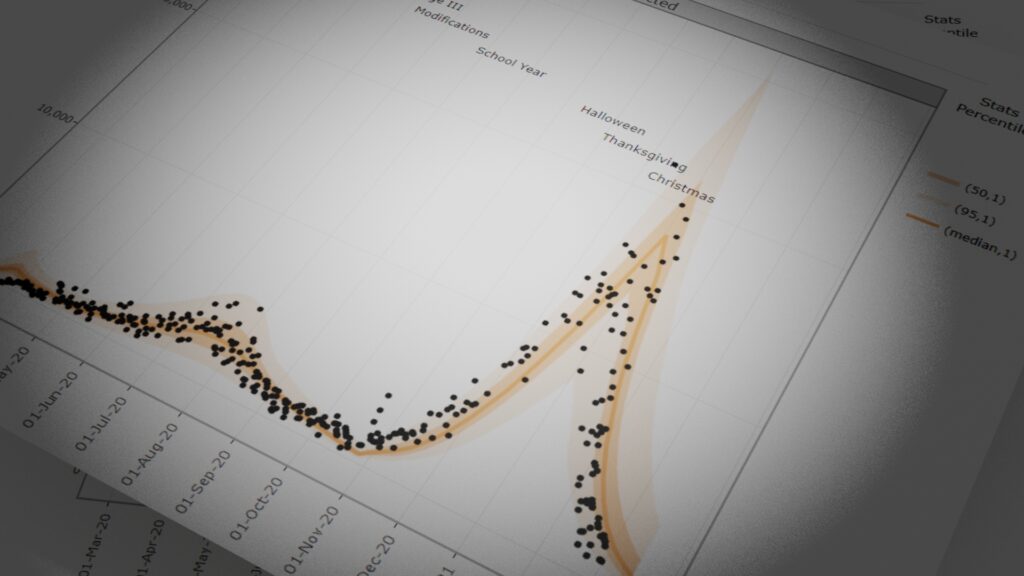
Epidemic dynamic models have provided estimates of key epidemic parameters important for policy planning throughout the evolving COVID-19 pandemic. However, currently implemented models have failed to investigate how these parameters differ across regions based on the prevalence of various combinations of key risk factors in the population, and how these differences in prevalence affect the dynamics of the epidemic in terms of impact on healthcare and spread of infection. Importantly, these models have also failed to investigate how the epidemic dynamics differ across racial and ethnic populations, across age, sex, and across cities.
Stay Connected Los Angeles: An innovative Public Health and the Arts Campaign to Mitigate the Impact of COVID-19
COVID-19 has exacerbated pervasive health disparities in the most vulnerable communities. Latinos in Los Angeles have the highest number of COVID-19 cases of all groups. To reach this population we propose to develop and test an intervention where arts meets public health. Working with local Latino artists in the Eastern part of Los Angeles, we seek to better understand health safety behaviors in this population via town hall meetings and focus groups, and develop and test educational materials, outdoor media materials and messaging to increase mitigation behaviors in the community. In addition to the campaign, a case management of resources interventions is being deployed with promotores de salud during a six weeks period to address the particular needs of highly vulnerable populations, including seniors, and those with chronic conditions. A community advisory committee of stakeholders will help to lead the project. Imagery and messaging will be displayed in the community as well as via partner agencies.
The Impact of COVID-19 on Food Insecurity in Los Angeles County

The COVID-19 pandemic has created a crisis in the U.S. food system and made disparities in food access and food security worse. Widespread food insecurity and hunger are severe threats to population health and national security.
Our multidisciplinary research team, under a strategic partnership with the Los Angeles County Emergency Food Security Branch, is evaluating the state of food insecurity in L.A. County during the pandemic. Our aim is to integrate innovative data sources that reflect the various features of our food system in order to and understand the broad impact of the COVID-19 pandemic on food insecurity in Los Angeles County.
Meeting with L.A. County experts on a weekly basis, the team has been answering pressing questions such as:
how has access to food and food insecurity changed?
what food and financial assistance programs are being accessed by people experiencing food insecurity, and are they effective?
how do the answers to these questions vary based on demographics and neighborhood location?
The research findings have informed L.A. County’s ongoing efforts to raise awareness of food assistance resources for residents in need and develop new programs. In the long term this research can help to chart a path for long-term strategies for food security and justice.
Rapid Antigen Testing as a Strategy to Reopen K-12 Schools

Rapid antigen testing is a promising strategy to prevent transmission of COVID by detecting and quarantining people who test positive. This study is examining the feasibility and effectiveness of using this technology as part of a comprehensive strategy to reopen K-12 schools. We will conduct qualitative interviews and focus groups of school administrators, teachers, parents, and students to understand logistical and attitudinal barriers and facilitators associated with using this technology. This information will be used to design a plan to use rapid antigen testing as part of a strategy to reopen schools. We will then conduct a pilot test of the strategy to evaluate its feasibility, effectiveness, and sustainability.
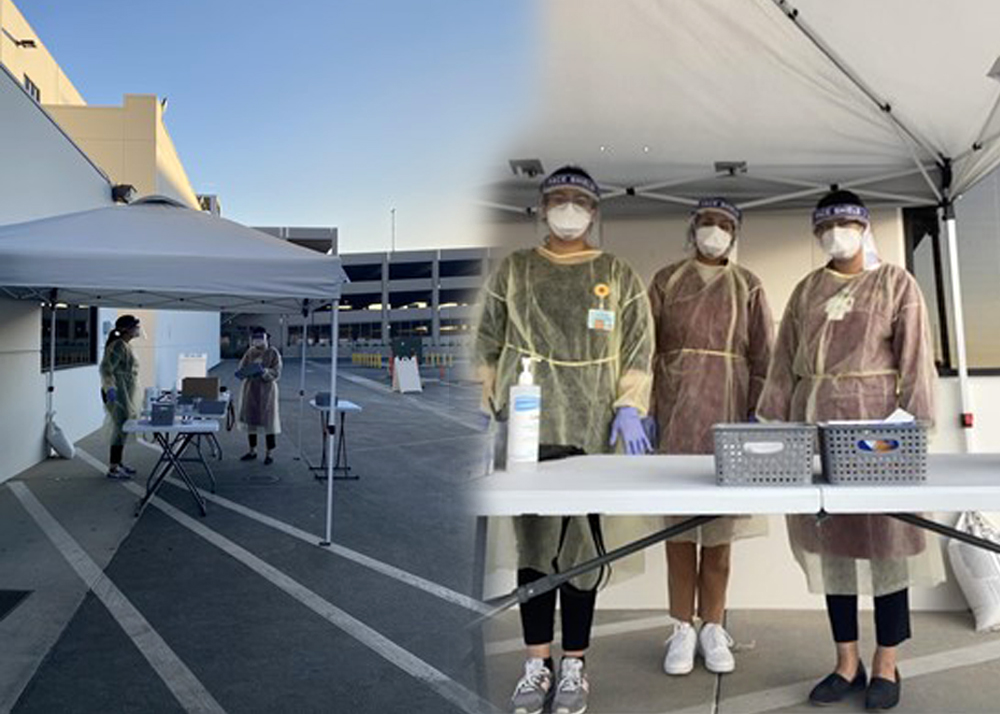
The Los Angeles Pandemic Surveillance Cohort Initiative

This project is a collaboration between the Population Health COVID-19 Pandemic Research Center (CPRC) initiative within the Department of Preventive Medicine, Keck School of Medicine of USC; the Price School of Public Policy/Schaeffer Center for Health Policy and Economics; and the Los Angeles County Department of Public Health (LACDPH). The overall goal is to generate data on the “true” prevalence of COVID-19 infection in LA County (overall, and among key subgroups) as well as its cumulative incidence (i.e., progression) over a defined period of time information that is crucial for planning and policy decisions. The approach being planned to achieve this goal is to recruit, with the assistance of a commercial provider that specializes in this activity, a community-based cohort of 2,000 households involving 2,000 adults (and, potentially, 1,000 associated children age 5 or greater) who are representative of the demographics of citizens in LA County, and who will consent to respond to a survey, participate in a drive-through protocol to gather “convenience” biological samples to test COVID-19 infection using a state-of-the-art antibody testing procedure (Wave 1), and then be surveyed and re-tested for antibodies again after 2-3 months (Wave 2). The current scope of work involves collection of data and samples in January-February, 2021; and the analysis of samples, data, and preliminary results related to Wave 1 by April, 2021. The associated protocol is also designed to incorporate, at minimal extra cost, labor, and inconvenience to the study participants, the gathering of additional information on the surveys and extra biological samples that will allow the investigative team to address additional goals and test hypotheses of important public health significance. The design will also establish the cohort as an on-going resource for generating additional evidence, based on maximum follow-up participation in additional surveys and testing, that addresses key questions of significance to public health policy.

